Introduction
Between 1974 and 2024, vaccination is estimated to have prevented 154 million deaths, including 146 million among children under the age of 5, of which 101 million were infants under 1 year old. Additionally, during this 50-year period, vaccination has contributed to the gain of 9 billion life-years and 10.2 billion years of full health. These achievements position vaccines and immunization as one of the most impactful healthcare interventions, second only, perhaps, to access to potable water.
In 2011, the WHO’s Strategic Advisory Group of Experts (SAGE) on Immunization established the Working Group on Vaccine Hesitancy, defining it as “complex and context-specific,” varying across time, place, and vaccine. By 2019, the WHO had identified vaccine hesitancy as one of the top 10 threats to global health.
International movements opposing science and vaccines have existed since the introduction of the smallpox vaccine. These movements emerge in waves, spreading rapidly and leaving behind a persistent “gray zone” of vaccine hesitancy. This hesitancy is counterbalanced only by scientific evidence and real-world data. Importantly, individuals in this gray zone—the vaccine-hesitant—represent a critical group. By addressing their concerns with accurate information and evidence-based communication, they can be guided toward acceptance, ultimately improving vaccination coverage and saving more lives.
This narrative review addresses vaccine hesitancy by examining five illustrative cases—smallpox, pertussis, measles, human papillomavirus (HPV), and SARS-CoV-2—followed by an analysis of underlying causes and potential interventions targeting this large “gray zone” of vaccine hesitancy, with an extensive focus on communication, and miscommunication.
Smallpox
Widespread smallpox vaccination began in the early 1800s, following Edward Jenner’s landmark cowpox experiments, which demonstrated that infection with cowpox lymph could protect against smallpox. Though revolutionary, Jenner’s ideas immediately faced public criticism.
The Vaccination Act of 1853 mandated vaccination for infants up to 3 months old, and the 1867 Act extended the requirement to children up to 14 years, imposing penalties for refusal. These laws fueled strong resistance, as many citizens demanded control over their own bodies and their children’s health. In response, the Anti-Vaccination League and the Anti-Compulsory Vaccination League emerged, alongside a surge of anti-vaccination journals.
The Leicester Demonstration (UK) in March of 1885 became one of the most infamous protests, drawing 80,000–100,000 demonstrators who paraded with banners, a child’s coffin, and an effigy of Jenner himself.
Pertussis:
Vaccination with diphtheria and tetanus toxoids combined with whole-cell pertussis (DTP) was introduced into the Expanded Program on Immunization (EPI) in 1974. By the early 1980s, mass vaccination had drastically reduced pertussis-related morbidity and mortality.
However, as the disease burden declined, public attention shifted toward concerns about vaccine safety. Reports of adverse events—widely covered by the media in the United States and the United Kingdom—led to reduced acceptance, and in some countries, complete rejection of whole-cell pertussis (wP) vaccines. Consequently, vaccination coverage dropped, precipitating major epidemics in 1977–79 and 1981–83, with over 65,000 cases and 12 deaths reported in 1978 alone.
In Japan, vaccination was suspended in 1975 following two suspected vaccine-related deaths and subsequent publicity. Within two years, pertussis incidence surged, resulting in approximately 40 deaths. These outbreaks underscore the serious consequences of declining coverage with an effective vaccine, with the true mortality likely underestimated due to under recognition of infant cases.
By the 1980s, widespread publicity linked wP vaccination to seizures and encephalopathy. Although subsequent studies (Jale et al., 1994; Barlow et al., 2001; Ray et al., 2006) conclusively refuted these associations, the damage was lasting—public mistrust persisted, and resistance to wP vaccination continues in some populations.
Measles and “the Wakefield fraud”
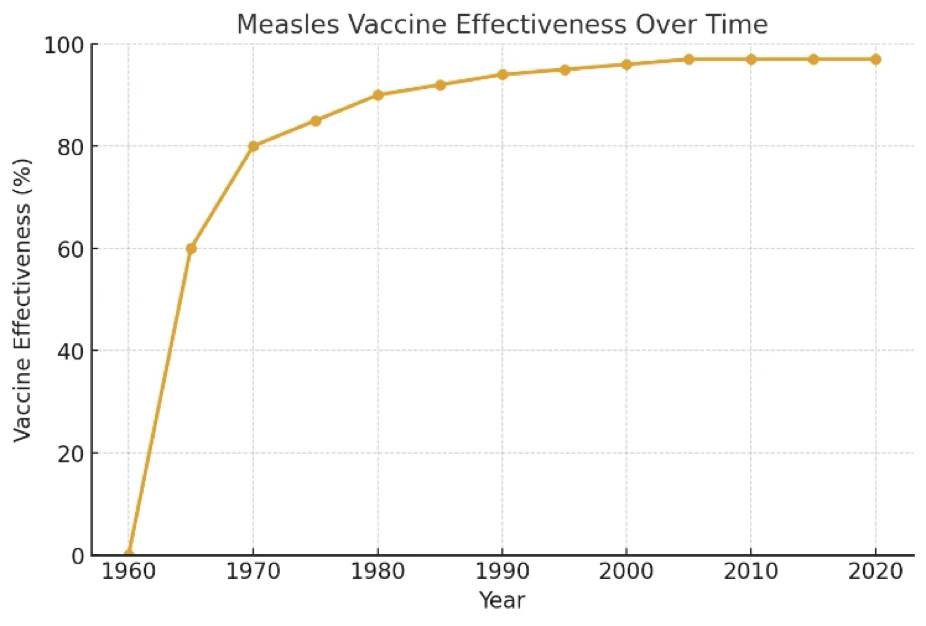
Between 1974 and 2024, measles vaccination alone is estimated to have saved over 97 million lives, the majority in children.
Nearly 25 years after the DTP controversy, vaccine skepticism re-emerged in England, this time targeting the measles, mumps, and rubella (MMR) vaccine. In 1998, Andrew Wakefield suggested a possible association between MMR vaccination, bowel disease, and autism. He later claimed the vaccine had not been adequately tested prior to widespread use. Media amplification of these claims fueled public fear and confusion about vaccine safety.
In 2004, The Lancet expressed regret for publishing Wakefield’s paper, and in 2010 formally retracted it after the UK General Medical Council found Wakefield guilty of serious professional misconduct, including undisclosed financial conflicts of interest. That same year, Wakefield was removed from the UK medical register. In 2011, the BMJ published investigative reports demonstrating that Wakefield had falsified data and sought to profit financially from his claims.
Since then, numerous high-quality studies have examined the safety of the MMR vaccine, and none have found any association with autism.
HPV Vaccination: Autoimmune Diseases, Sexuality, and Other Concerns
Extensive research has assessed the potential association between HPV vaccination and autoimmune or neurological disorders. Collectively, these studies included over 3 million adult women, nearly 1 million adolescent girls, 600,000 boys, and more than 250,000 younger girls. While small signals have been reported for conditions such as Raynaud’s disease, type 1 diabetes, vitiligo, and narcolepsy, no causal link with HPV vaccination has been established.
A common parental concern is whether vaccination between ages 9 and 12 is necessary, as children are not yet sexually active. Questions about potential promotion of early sexual activity or promiscuity frequently arise. However, evidence consistently shows that HPV vaccination does not alter sexual behavior. Importantly, vaccination prior to sexual debut provides the greatest protection, as HPV exposure can occur soon after first sexual contact, and the timing of this varies across individuals, cultures, and countries. Moreover, while HPV is primarily transmitted sexually, non-sexual transmission—via fomites, shared clothing, horizontal, and even vertical routes—has also been reported. Vaccination at younger ages ensures durable immunity before exposure, making early immunization (starting at age 9) optimal. In this context, it is possible to vaccinate too late, but never too early.
Another misconception is that HPV vaccination may cause ovarian failure. A large 2018 study of nearly 20,000 women aged 11–34 found no association between adolescent HPV vaccination and ovarian failure, reaffirming the vaccine’s safety.
COVID-19 Vaccination: From Preventing Millions of Deaths to Fears of the Vaccine Itself
Between 2020 and 2024, COVID-19 vaccination is estimated to have prevented 2.53 million deaths worldwide—equivalent to one life saved for every 5,400 doses administered. Approximately 82% of these lives were saved through vaccination prior to viral exposure. Notably, 57% of prevented deaths occurred during the Omicron phase, and 90% were among individuals aged ≥60 years. In total, vaccination preserved an estimated 14.8 million years of life, corresponding to one year of life saved for every 900 doses delivered.
Despite this impact, the rollout of COVID-19 vaccines coincided with the rise of “health freedom” political activism, particularly within far-right movements in the United States. This movement discouraged vaccination, contributing to an estimated 200,000 preventable deaths among unvaccinated Americans in 2021–2022. Antivaccine activism has since emerged as a major lethal force in that country.
Globally, vaccine confidence has also declined. In the UK, the proportion of adults who believed vaccines were safe and effective fell from 90% in 2018 to 70% in 2023, according to the Vaccine Confidence Project (London School of Hygiene and Tropical Medicine). A similar downward trend was observed in 52 of 55 countries surveyed since 2019. Complementary polling by YouGov found that the share of adults who believe vaccines have undisclosed harmful side effects rose from 19% in 2019 to 30% in 2024.
Internet age and misinformation
Since the emergence of social media in the early 2000s, concerns have grown about the rapid spread of health-related rumors and misinformation. Surveys conducted by the UK Health Security Agency, U.S. institutions, and others report that 20–30% of parents encountered online content that made them question vaccines—a sharp increase from just 6% the previous year.
As social media platforms evolved from niche communities into central components of the global media landscape, the dynamics of misinformation shifted dramatically. Now somebody in one corner of the world can post something and, within seconds, millions elsewhere can see it. It is not just the speed, but also the unprecedented reach of misinformation that puts us in entirely uncharted territory.
Politics
Recent political shifts within federal health leadership have raised concerns about the influence of antivaccination rhetoric in major countries’ health agencies. Changes in advisory committee composition, including the replacement of scientific experts with individuals linked to antivaccine activism or potential conflicts of interest, mark a departure from prior evidence-based practice.
These developments illustrate how political decisions can shape public health policy and communication. The risk is that antivaccination sentiment may gain greater visibility and legitimacy, both domestically and internationally. If questionable or low-quality science is promoted through official channels, it could undermine trust in federal health institutions, complicate science communication, and contribute to vaccine hesitancy worldwide.
Exploring Solutions to Vaccine Hesitancy
Measuring vaccine hesitancy is key. Because directly “combating” antivaccine movements is not feasible, efforts should instead focus on understanding the population-specific drivers of vaccine uptake. This requires distinguishing between vaccine hesitancy and external barriers such as access.
Several new tools are being developed to address this need. The Vaccine Barriers Assessment Tool, for example, is designed to evaluate both acceptance- and access-related barriers to childhood vaccination in Australia and New Zealand, with potential for adaptation to other contexts, including low- and middle-income countries and across different populations (e.g., school-age children, adults) and vaccines (e.g., influenza, COVID-19). Similarly, the World Health Organization’s Working Group on the Behavioral and Social Drivers of Vaccination is developing standardized quantitative and qualitative instruments to measure these drivers globally.
Such tools can help detect emerging trends in vaccine accessibility and acceptance. Critically, understanding why specific groups or individuals fail to receive recommended vaccines is essential for designing and evaluating cost-effective, tailored strategies to improve uptake.
Communication and community engagement
Research confirms provider recommendation to vaccinate is one of the key drivers of vaccine uptake, with different approaches taken by providers. Presumptive communication assumes people are ready to vaccinate (“We’re going to be …”), whereas participatory communication asks people if they want to vaccinate (“Did you want to …”). Studies have suggested a presumptive approach is associated with higher uptake of childhood vaccines (observational studies) or adolescent HPV vaccines (randomized controlled trial).
Motivational interviewing offers a more structured counseling approach designed to guide people towards change by exploring and enhancing internal motivation.
In recent years, a growing number of entities have misrepresented themselves as scholarly journals, seeking financial gain without adhering to accepted standards of academic publishing. The proliferation and increasing boldness of these predatory outlets highlights the urgent need to expose their practices and to consider concrete actions that stakeholders can take to counter their deceptive activities.
Data vs. sentiments
Sentiment analysis is one of the most widely studied applications in Natural Language Processing (NLP). It enables the computation of sentiment scores, transforming large volumes of unstructured text into structured, quantifiable opinions. A common approach involves counting the number of positive and negative words in a document to derive an overall sentiment score. Typically, each positive word contributes +1, while negative words contribute −1, depending on the chosen method (Qorib M, et al.).
The Relative Proportional Difference (RPD) ranges from −1 to 1 and is defined as:
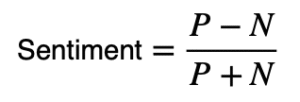
where P denotes the number of positive words and N the number of negative words in the text.
Let us now insert the variables based on the reader’s perspective:
- Scientist perspective: “A blog is not equivalent to a scientific publication, and the reported RPD is not well measured.”
- Non-scientist perspective (A): “The RPD is 0.5 (<1), but I would like to see the proportions and the ‘intensity’ of toxicity.”
- Non-scientist perspective (B): “The RPD is 0.5 (<1); this suggests the vaccine is more toxic than effective. However, I would like to know more about the source mentioned in the blogs.”
- Non-scientist perspective (C): “The RPD is 0.5 (<1), so the vaccine is evidently more toxic than effective.”
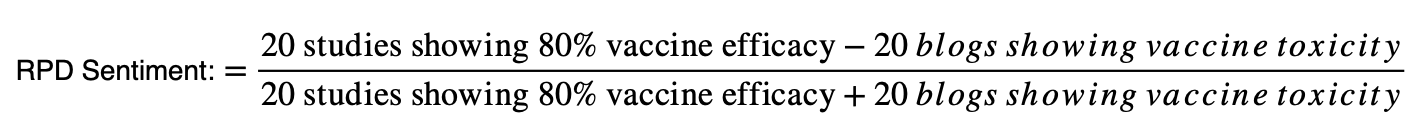
For now, let us set aside the algebra and simply present these two variables. Both the graph and the image are intended only as illustrative tools for the purposes of this column.
A plot:
Measles real-life effectiveness over time, published by WHO
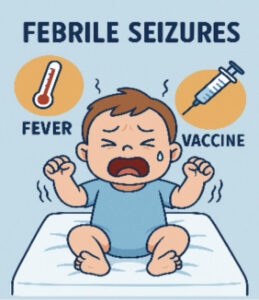
And an image
A case of febrile seizures in a child, erroneously attributed by the author to the measles vaccine.
- Scientist perspective: “The plot clearly demonstrates that the measles vaccine is effective. The baby’s febrile seizures are most likely the result of an acute viral infection, not the vaccine.”
- Non-scientist perspective (A): “I can see that the measles vaccine appears effective, but it still seems like it can cause a baby to develop seizures.”
- Non-scientist perspective (B): “The idea of having a baby with seizures most likely caused by the vaccine is terrible, and I do not understand the plot.”
- Non-scientist perspective (C): “Data can always be manipulated, but the baby with seizures is real.”
The rise of instant information, the decline of sustained critical thinking
Over the past decade, the volume of available information has grown exponentially; however, much of it is generated by unverified sources and delivered in short formats, such as blogs or clips lasting only one to two minutes. Younger audiences, in particular, are more likely to consume these brief messages than to engage with longer, evidence-based explanations. This trend is shaping the thinking of millions, discouraging both self-criticism and external scrutiny of the information received—largely because such critical processes require time and effort, and may even force us to confront how media organizations manipulate public perception.
This phenomenon is closely tied to emotions, which are triggered more rapidly than rational thought. As a result, emotionally charged content often outpaces reflective reasoning, making individuals more vulnerable to misinformation. Recognizing these dynamic highlights the importance of fostering critical thinking and promoting evidence-based communication, so that voices are raised in support of facts rather than falsehoods.
Vaccine fatigue
Vaccine fatigue can be defined as inaction toward vaccine information, instructions, or recommendations, often resulting from perceived burden or burnout. This phenomenon became globally evident during the COVID-19 pandemic. Several antecedents have been identified, including:
- High frequency of immunization demands
- Misconceptions regarding disease severity and the need for vaccination
- Concerns about vaccine side effects
- Lack of trust in government and media
A comprehensive understanding of these factors can help governments and health authorities design more effective countermeasures to limit the impact of vaccine fatigue. By addressing these drivers, societies can reduce the risk of escalating vaccine fatigue into outright vaccine hostility, ultimately supporting stronger and more sustainable immunization programs.
Conclusions
Vaccine hesitancy is dynamic and continuously evolving—an issue made particularly visible during the COVID-19 pandemic. To address it effectively, open and ongoing dialogue about vaccination is essential to identify and respond to emerging concerns early. Physicians and other health care providers remain among the most trusted sources of medical advice, but overcoming mistrust also requires deeper understanding of the roots of misinformation, misperceptions, and contextual barriers.
Meeting this challenge calls for country- and region-specific policies and protocols, reinforced by skilled science communicators, to build trust and promote evidence-based reasoning over emotionally charged, unscientific, and potentially harmful misinformation. For these efforts to succeed, strategies must be consistent, proportionate, and easily understood, ensuring stronger and more resilient public health systems.
Biblography:
Tuckerman J, Kaufman J, Danchin M. Effective Approaches to Combat Vaccine Hesitancy. Pediatr Infect Dis J. 2022 May 1;41(5):e243-e245. doi: 10.1097/INF.0000000000003499.
The College of Physicians of Philadelphia: History of Anti-vaccination movements. Accessed October 14, 2025. https://historyofvaccines.org/vaccines-101/misconceptions-about-vaccines/history-anti-vaccination-movements.
Laine C, Babski D, Bachelet VC, Bärnighausen TW, Baethge C, Bibbins-Domingo K, Frizelle F, Gollogy L, Kleinert S, Loder E, Monteiro J, Rubin EJ, Sahni P, Wee CC, Yoo JH, Zakhama L; the International Committee of Medical Journal Editors (ICMJE). Predatory Journals: What Can We Do to Protect Their Prey? Dtsch Arztebl Int. 2025 Jan 24;122(2):31-32. doi: 10.3238/arztebl.m2024.0263.
BBC: The strange history of the anti-vaccine movement. Accessed October 13, 2025. https://www.bbc.com/future/article/20250905-the-strange-history-of-the-anti-vaccine-movement.
Wikipedia: MMR autism fraud. Accessed October 14, 2025. https://en.wikipedia.org/wiki/Lancet_MMR_autism_fraud.
Our world in data: measles vaccines save millions of lives each year. Accessed: October 16, 2025. https://ourworldindata.org/measles-vaccines-save-lives.
Taumberger N, Joura EA, Arbyn M, Kyrgiou M, Sehouli J, Gultekin M. Myths and fake messages about human papillomavirus (HPV) vaccination: answers from the ESGO Prevention Committee. Int J Gynecol Cancer. 2022 Oct 3;32(10):1316-1320. doi: 10.1136/ijgc-2022-003685.
SchiTechDaily: 2.5 millions lives saved: the untold story of COVID-19 vaccines’ global impact. Accessed October 16, 2025. https://scitechdaily.com/2-5-million-lives-saved-the-untold-story-of-covid-vaccines-global-impact/.
BBC: Rise of vaccine distrust – why more of us are questioning jabs. Accessed October 18, 2025. https://www.bbc.com/news/articles/c1jgrlxx37do.
Dhaliwal D, Mannion C. Antivaccine Messages on Facebook: Preliminary Audit. JMIR Public Health Surveill. 2020 Oct 20;6(4):e18878. doi: 10.2196/18878.
Kaplan S, von Isenburg M, Waldrop L. Prepandemic Antivaccination Websites’ COVID-19 Vaccine Behavior: Content Analysis of Archived Websites. JMIR Form Res. 2023 Jan 11;7:e40291. doi: 10.2196/40291.
Ngai CSB, Singh RG, Yao L. Impact of COVID-19 Vaccine Misinformation on Social Media Virality: Content Analysis of Message Themes and Writing Strategies. J Med Internet Res. 2022 Jul 6;24(7):e37806. doi: 10.2196/37806.
Jamison A, Broniatowski DA, Smith MC, Parikh KS, Malik A, Dredze M, Quinn SC. Adapting and Extending a Typology to Identify Vaccine Misinformation on Twitter. Am J Public Health. 2020 Oct;110(S3):S331-S339. doi: 10.2105/AJPH.2020.305940.
Herrera-Peco I, Jiménez-Gómez B, Romero Magdalena CS, Deudero JJ, García-Puente M, Benítez De Gracia E, Ruiz Núñez C. Antivaccine Movement and COVID-19 Negationism: A Content Analysis of Spanish-Written Messages on Twitter. Vaccines (Basel). 2021 Jun 15;9(6):656. doi: 10.3390/vaccines9060656.
Kirkland A, Greer SL. The antivaccine movement threatens health in the US and worldwide. BMJ. 2025 Jul 3;390:r1383. doi: 10.1136/bmj.r1383.
Qorib M, Oladunni T, Denis M, Ososanya E, Cotae P. Covid-19 vaccine hesitancy: Text mining, sentiment analysis and machine learning on COVID-19 vaccination Twitter dataset. Expert Syst Appl. 2023 Feb;212:118715. doi: 10.1016/j.eswa.2022.118715.
Stolle LB, Nalamasu R, Pergolizzi JV Jr, Varrassi G, Magnusson P, LeQuang J, Breve F; NEMA Research Group. Fact vs Fallacy: The Anti-Vaccine Discussion Reloaded. Adv Ther. 2020 Nov;37(11):4481-4490. doi: 10.1007/s12325-020-01502-y.
Horowitz ME. The Vaccine-Hesitant Moment. N Engl J Med. 2022 Sep 15;387(11):1050. doi: 10.1056/NEJMc2210367.
Su Z, Cheshmehzangi A, McDonnell D, da Veiga CP, Xiang YT. Mind the “Vaccine Fatigue”. Front Immunol. 2022 Mar 10;13:839433. doi: 10.3389/fimmu.2022.839433. Erratum in: Front Immunol. 2023 Jan 04;13:1122354. doi: 10.3389/fimmu.2022.1122354.
Nursing Central: Vaccine fatigue: a new phenomenon. Accessed October 18, 2025. https://nursingcecentral.com/vaccine-fatigue/.
van Reijmersdal EA, Fransen ML, van Noort G, Opree SJ, Vandeberg L, Reusch S, van Lieshout F, Boerman SC. Effects of Disclosing Sponsored Content in Blogs: How the Use of Resistance Strategies Mediates Effects on Persuasion. Am Behav Sci. 2016 Nov;60(12):1458-1474. doi: 10.1177/0002764216660141.
Islam MS, Kamal AM, Kabir A, Southern DL, Khan SH, Hasan SMM, Sarkar T, Sharmin S, Das S, Roy T, Harun MGD, Chughtai AA, Homaira N, Seale H. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021 May 12;16(5):e0251605. doi: 10.1371/journal.pone.0251605.
De Giorgio A, Kuvačić G, Maleš D, Vecchio I, Tornali C, Ishac W, Ramaci T, Barattucci M, Milavić B. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines (Basel). 2022 Mar 21;10(3):481. doi: 10.3390/vaccines10030481.
Powell GA, Zinszer K, Verma A, Bahk C, Madoff L, Brownstein J, Buckeridge D. Media content about vaccines in the United States and Canada, 2012-2014: An analysis using data from the Vaccine Sentimeter. Vaccine. 2016 Dec 7;34(50):6229-6235. doi: 10.1016/j.vaccine.2016.10.067.
Ebrahimi OV, Johnson MS, Ebling S, Amundsen OM, Halsøy Ø, Hoffart A, Skjerdingstad N, Johnson SU. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front Public Health. 2021 Jul 1;9:700213. doi: 10.3389/fpubh.2021.700213.
Orhan A. Fake news detection on social media: the predictive role of university students’ critical thinking dispositions and new media literacy. Smart Learn Environ. 2023;10(1):29. doi: 10.1186/s40561-023-00248-8.
Hodge JG Jr. Legal Underpinnings of the Great Vaccine Debate of 2025. J Law Med Ethics. 2025 Mar 27;53(1):1-5. doi: 10.1017/jme.2025.51.
Genetic Literacy Project (Science, not ideology): Vaccines, politics, and the fragile future of public health.
MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161-4. doi: 10.1016/j.vaccine.2015.04.036.
WHO, January 2025: Summary of SAGE-WHO conclusions and recommendations on vaccine hesitancy. Accessed October 2, 2025. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.who.int/docs/default-source/immunization/demand/summary-of-sage-vaccinehesitancy-en.pdf?sfvrsn=abbfd5c8_2.
Chacon-Cruz E, Lopatynsky-Reyes EZ, Maithal K, Bakeera-Kitaka S, Ankunda C, Casellas J, Vir Singh M, Nikiema F, Sheku M, Zazueta OE. Vaccination against Pertussis in the era of acellular and whole-cell vaccines. Medical Research Archives 2024; 12(3): 1-18. DOI: https://doi.org/10.18103/mra.v12i3.5126.
Carpiano RM, Callaghan T, DiResta R, Brewer NT, Clinton C, Galvani AP, Lakshmanan R, Parmet WE, Omer SB, Buttenheim AM, Benjamin RM, Caplan A, Elharake JA, Flowers LC, Maldonado YA, Mello MM, Opel DJ, Salmon DA, Schwartz JL, Sharfstein JM, Hotez PJ. Confronting the evolution and expansion of anti-vaccine activism in the USA in the COVID-19 era. Lancet. 2023 Mar 18;401(10380):967-970. doi: 10.1016/S0140-6736(23)00136-8.
Houston Public Media, September 15, 2025: Dr. Peter Hotez: How to fight back in the war on science. Accessed October 18, 2025. https://www.houstonpublicmedia.org/articles/news/2025/09/15/530877/dr-peter-hotez-how-to-fight-back-in-the-war-on-science/.
Kaufman J, Tuckerman J, Bonner C, Durrheim DN, Costa DSJ, Trevena L, Henseler J, Danchin M. Development and validation of the Vaccine Barriers Assessment Tool for identifying drivers of under-vaccination in children under five years in Australia. Hum Vaccin Immunother. 2024 Dec 31;20(1):2359623. doi: 10.1080/21645515.2024.2359623.







