Introduction:
Scientific interest in the etiological links between infectious diseases and cancer has been steadily increasing for several reasons:
- A growing number of neoplasms have been definitively associated with specific pathogens.
- Research into the pathways leading to carcinogenesis has illuminated critical cellular processes.
- Perhaps most importantly, cancers caused by infections are, in principle, preventable—either at the primary level by blocking infection (e.g. vaccination) or secondarily by interrupting the carcinogenic process. This rationale underpins two of the most impactful public health campaigns of recent decades: vaccination against hepatitis B virus and human papillomavirus.
Cancer remains as a pandemic, not only because of its immense burden in morbidity, mortality, and economic cost, but also due to the complexity of its evolution and the challenges in developing effective treatments. Its burden is magnified by the fact that “cancer” encompasses a constellation of diseases, each with distinct pathogenic mechanisms and prognoses. Within this spectrum, cancers that arise directly from infectious processes hold particular significance for two reasons. First, unraveling how infections drive malignant transformation provides insights into fundamental cellular pathways of carcinogenesis. Indeed, viruses have been described as infectious agents capable of driving cellular transformation toward dysplasia, and anaplasia. Unlike many environmental risk factors, infections are discrete, traceable events, often with measurable burden, that can be systematically studied over time. Second, infection-related cancers are inherently preventable—whether through primary measures such as vaccination or through secondary approaches that target chronic infections before they progress to malignancy.
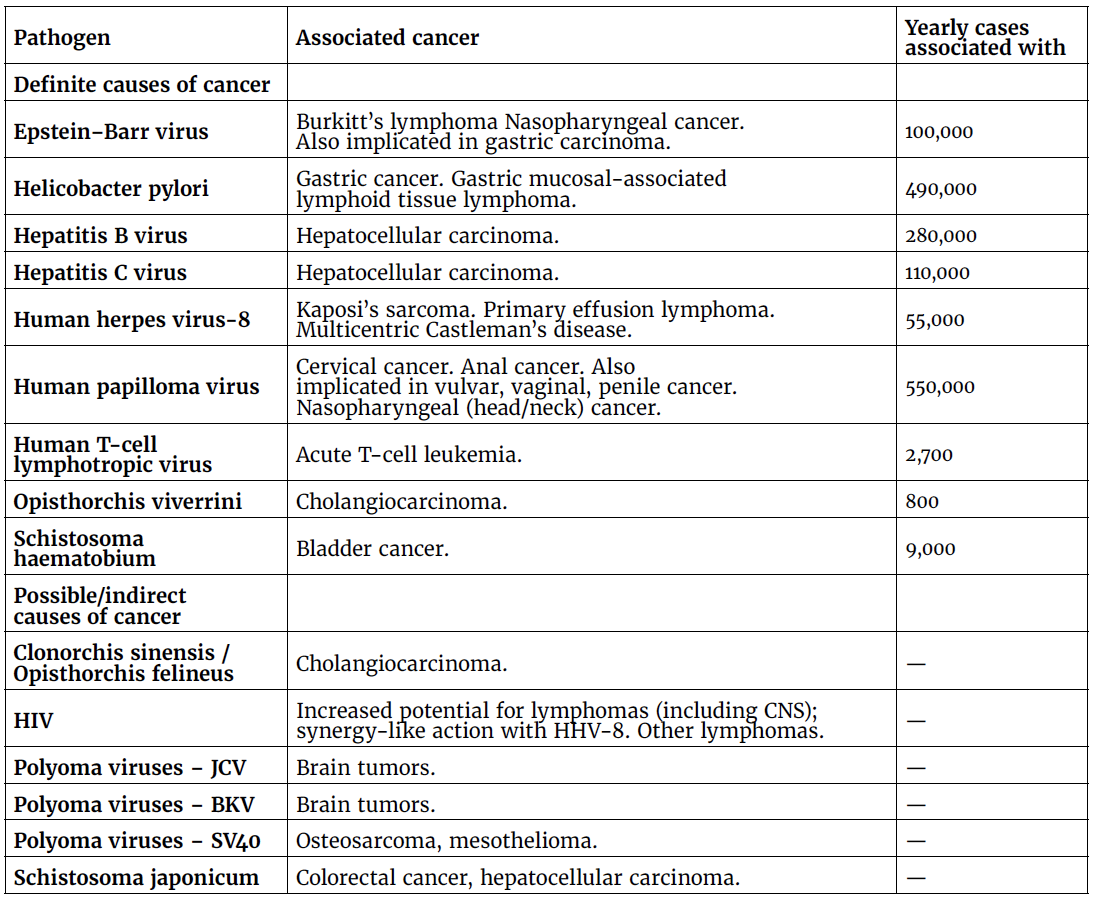
Infectious agents as confirmed and/or potential contributors to cancer:
The list of infectious agents linked to carcinogenesis—whether definitively or speculatively—continues to expand, with additional neoplasms being associated with recognized oncogenic pathogens. A classic example is Epstein–Barr virus (EBV), which, beyond its established role in Burkitt’s lymphoma is also etiologically implicated in other malignancies. Perhaps even more illustrative is its association with nasopharyngeal carcinoma, alongside the role of human papillomavirus (HPV).
Table 1. Pathogens with a definitive and possible or indirect role in cancer causation.
(Taken from Pappas G. Clin Microbiol Infect. 2009 Nov;15(11):961-3.)
Additionally, a retrospective cohort study conducted in Germany evaluated individuals vaccinated against HPV at age 8 years or older, who were propensity score–matched to unvaccinated controls. Outcomes included the incidence of malignancies in the head and neck, gastrointestinal, anogenital, neuronal, and hematologic systems, as well as all-cause mortality, assessed over 8- and 20-year follow-up periods. Kaplan–Meier survival analysis and hazard ratios (HRs) were applied. HPV vaccination was significantly associated with reduced risks of hypopharyngeal and laryngeal carcinomas (8-year HR: 0.19; 95% CI: 0.057–0.631; p = 0.0025; 20-year HR: 0.227; 95% CI: 0.067–0.764; p = 0.0092) and leukemia (8-year HR: 0.461; p = 0.0035; 20-year HR: 0.443; p = 0.0019). No significant protection was observed for rectal, anal, oral cavity, or prostate cancers. Importantly, all-cause mortality was reduced by nearly half among vaccinated individuals (8-year HR: 0.543; 20-year HR: 0.536; both p < 0.0001). Beyond epithelial malignancies, these findings indicate that HPV vaccination may confer systemic cancer protection, particularly in hematologic and possibly neuronal tissues. This suggests a broader biological impact of HPV vaccination than previously recognized and underscores the need for mechanistic studies to elucidate HPV’s oncogenic pathways. If confirmed, these results could support the expansion of HPV vaccination strategies to broader indications and wider population coverage.
To date, only two viral vaccines are globally administered with the main purpose of decreasing cancer:
- Hepatitis B: World Hepatitis Day has been celebrated on July 28 since 2010, a date chosen in honor of the birthday of Dr. Baruch Blumberg, winner of a Nobel Prize for discovering the hepatitis B virus and developing its diagnostic test and vaccine. Each year, this date reinforces the need to intensify national and international efforts to eliminate viral hepatitis. For 2025, the global campaign adopts the theme “Hepatitis: Let’s break it down!” which calls on governments, civil society, and partners to dismantle financial, social, and systemic barriers, including stigma, that hinder access to hepatitis prevention, diagnosis, and treatment, as well as liver cancer prevention. The focus of the efforts coordinated by the World Health Organization (WHO) and the Pan American Health Organization (PAHO) is on simplifying, expanding, and integrating vaccination services, safe practices, harm reduction, testing, and treatment into national health systems. Estimates from the WHO indicate that in 2022, approximately 254 million people were living with hepatitis B and 50 million with hepatitis C, causing approximately 1.3 million deaths annually, many of them from cirrhosis and liver cancer. According to multilateral health agencies, it is possible to prevent 2.8 million deaths by 2030, but only if countries act now. The elimination of hepatitis is within our reach, as well as decreasing significantly all hepatitis B-related hepatocarcinoma cases.
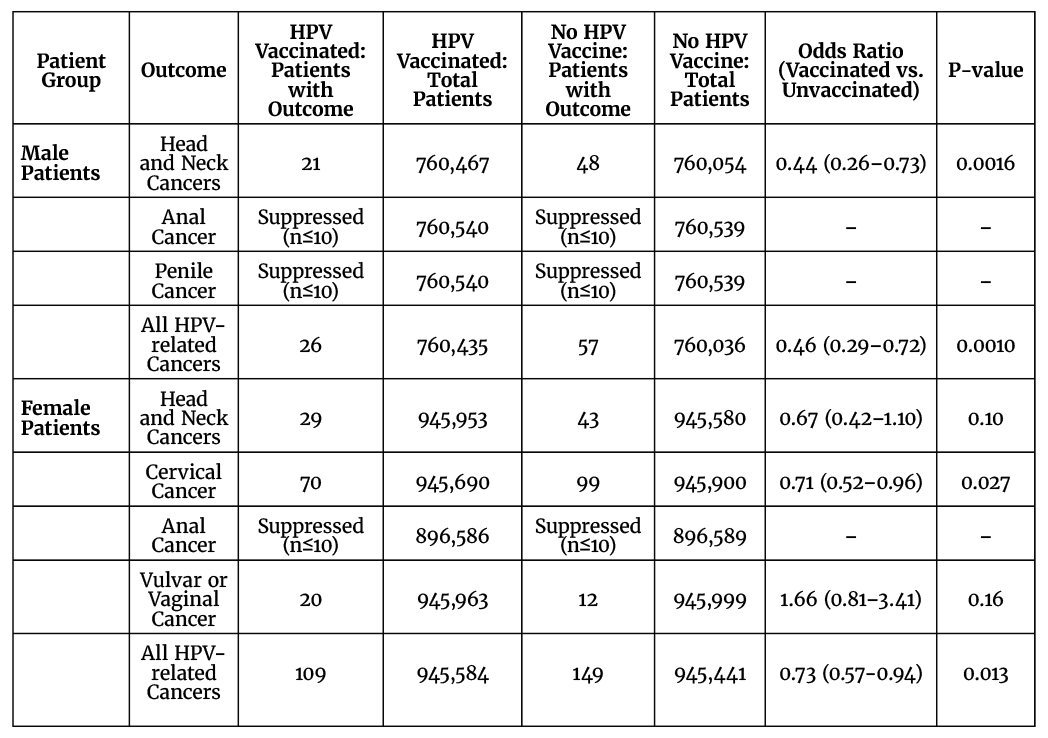
- HPV: An American retrospective cohort study was conducted using a patient population selected from the TriNetX United States Collaborative Network. Patients 9-39 years old attending medical encounters where any vaccine was administered between 1/1/2010 and 12/31/2023 were divided into two cohorts: patients vaccinated for HPV at least five years prior and those no history of HPV vaccination. The results were impressive, vaccination vs. HPV significantly reduced not only cervical cancer in women, but also anal and head/neck cancer in both genders, as well as penile cancer in males.
shown in Table 2.
Table 2. Effects of HPV vaccination on the development of HPV-related cancers: A retrospective analysis of a United States-based cohort.
(Taken from Dekloe J, et al. J Clin Oncol 2024; 42 (Suppl 16): Abstract 10507).
Respiratory viruses and cancer risk:
Recent evidence suggests that respiratory viruses may play a role in triggering cancer, a finding that carries important implications for both improving vaccination coverage and accelerating research and development of new vaccines against these pathogens.
In a murine model, phenotypic transitions and cellular expansions were shown to be interleukin-6–dependent. The study demonstrated that dormant disseminated cancer cells (DCCs) impair lung T cell activation, while CD4⁺ T cells promote pulmonary metastatic burden following influenza infection by suppressing CD8⁺ T cell activation and cytotoxicity.
Crucially, these experimental findings are consistent with human observational data. Analyses of cancer survivors from the UK Biobank (all cancer types) and Flatiron Health (breast cancer) databases revealed that SARS-CoV-2 infection significantly increases the risk of cancer-related mortality and lung metastasis compared with uninfected cancer survivors.
Additionally, DeGregori and colleagues explored whether acute inflammation triggered by a respiratory infection could reactivate dormant cancer cells. To investigate this, they genetically engineered mice to develop breast tumors resembling those in humans and to harbor dormant tumor cells in other tissues, including the lungs. The animals were then infected with either SARS-CoV-2 or influenza. Within days, the dormant cancer cells in the lungs became highly active, proliferating and forming metastatic lesions. Interestingly, it wasn’t the viruses themselves driving this process. The researchers identified a key immune molecule, interleukin-6 (IL-6), which amplifies the body’s response to threats, as the main culprit. When they engineered mice to lack IL-6, the dormant cancer cells multiplied far more slowly. About two weeks after infection, the cells returned to a dormant state. These findings suggest that respiratory infections do not directly cause cancer. Instead, they can create conditions—through inflammation—that make it more likely for dormant cancer cells to reactivate in response to future threats, such as subsequent infections or genetic mutations.
Conclusions:
By linking a specific neoplasia to a particular infectious agent, researchers have highlighted a clear path for prevention: eliminating the initiating infection or its carcinogenic effects. This approach has naturally attracted significant scientific attention and underpins some of the most promising public health campaigns aimed at reducing both the incidence and mortality of various malignancies. A recent and notable example is HPV and the challenges and opportunities arising from the recent implementation of mass vaccination programs.
Furthermore, respiratory virus infections can promote the awakening and expansion of previously seeded dormant cancer cells.
All of this underscores the need for vaccinology to not only increase coverage for vaccines against hepatitis B, HPV, SARS-CoV-2, and influenza, but also to drive research into the links between infections and cancer. It highlights the importance of investing in both basic research on these associations and the development of new vaccines. Indeed, the field of vaccinology extends far beyond the control of infectious diseases alone.
Bibliography:
- Dresden BP, Alcorn JF. Inflammation during viral infection can rouse dormant cancer cells. Nature. 2025 Jul 30. doi: 10.1038/d41586-025-02137-1.
- Pappas G. Infectious causes of cancer: an evolving educational saga. Clin Microbiol Infect. 2009 Nov;15(11):961-3. doi: 10.1111/j.1469-0691.2009.03034.x.
- Bireme/PAHO/WHO Bulletin: Global mobilization against viral hepatitis. Last accessed Sept 10, 2025. https://boletin.bireme.org/en/2025/07/31/july-28-global-mobilization-against-viral-hepatitis/.
- Christian Seebauer, Mohamed Faluogy, Peter Sieg, Henning Olbrich, Ralf Ludwig. HPV vaccination and malignancy risks beyond cervical cancer: A retrospective global cohort study. Pharmacological Research. 2025; 218: 107851. https://doi.org/10.1016/j.phrs.2025.107851.
- WHO: Immunizing against HPV. Last accessed Sept 10, 2025. https://www.who.int/activities/immunizing-against-hpv.
- Chia SB, Johnson BJ, Hu J, Valença-Pereira F, Chadeau-Hyam M, Guntoro F, Montgomery H, Boorgula MP, Sreekanth V, Goodspeed A, Davenport B, De Dominici M, Zaberezhnyy V, Schleicher WE, Gao D, Cadar AN, Petriz-Otaño L, Papanicolaou M, Beheshti A, Baylin SB, Guarnieri JW, Wallace DC, Costello JC, Bartley JM, Morrison TE, Vermeulen R, Aguirre-Ghiso JA, Rincon M, DeGregori J. Respiratory viral infections awaken metastatic breast cancer cells in lungs. Nature. 2025 Jul 30. doi: 10.1038/s41586-025-09332-0.
- Dekloe J, et al. Effects of HPV vaccination on the development of HPV-related cancers: A retrospective analysis of a United States-based cohort. J Clin Oncol 2024; 42 (Suppl 16): Abstract 10507. https://doi.org/10.1200/JCO.2024.42.16_suppl.10507.
- WHO: Hepatitis B. Last accessed September 9, 2025. https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
- Galluzzi L, Buqué A, Kepp O, Zitvogel L, Kroemer G. Immunogenic cell death in cancer and infectious disease. Nat Rev Immunol. 2017 Feb;17(2):97-111. doi: 10.1038/nri.2016.107.
- Kimura M, Kothari S, Gohir W, Camargo JF, Husain S. MicroRNAs in infectious diseases: potential diagnostic biomarkers and therapeutic targets. Clin Microbiol Rev. 2023 Dec 20;36(4):e0001523. doi: 10.1128/cmr.00015-23.