Authors:
Enrique Chacon-Cruz, M.D., MSc
Felicitas Colombo, MPA
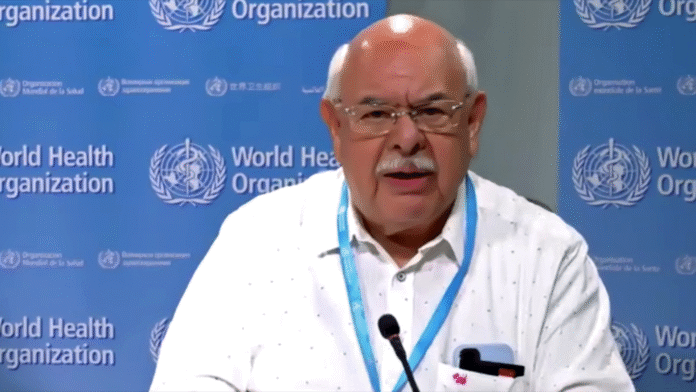
Prof. Alejandro Cravioto is a distinguished physician, researcher, and global health leader with decades of experience in medical education, pediatric infectious diseases, and vaccine development. He currently serves as a Professor at the Faculty of Medicine of the National Autonomous University of Mexico (UNAM) in Mexico City, where he also earned his medical degree with honors. Prof. Cravioto completed his specialization in Pediatrics at the National Institute of Pediatrics in Mexico City, and furthered his academic training at the London School of Hygiene and Tropical Medicine, University of London, where he obtained a Diploma in Tropical Public Health and a Ph.D.
From 1995 to 2003, Prof. Cravioto served as Dean of the Faculty of Medicine at UNAM, where he played a pivotal role in advancing medical education, research infrastructure, and academic exchange. Following his tenure in academic leadership in Mexico, he took on an influential global role as Executive Director of the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) from 2005 to 2012. Under his leadership, icddr,b strengthened its position as one of the world’s premier research institutions focused on infectious diseases, nutrition, and child health.
From 2012 to 2014, Prof. Cravioto served as Chief Scientific Officer at the International Vaccine Institute (IVI) in Seoul, Republic of Korea, where he contributed to the institute’s mission to develop and deliver safe, effective, and affordable vaccines for people in developing countries.
Prof. Cravioto’s primary research interests have centered on the interaction between infection and growth in infants and young children, and the molecular pathogenesis of enteric bacterial infections. His groundbreaking work on Enterotoxigenic and Enteropathogenic Escherichia coli (ETEC and EPEC) has significantly advanced the understanding of diarrheal disease and laid the scientific foundation for the development of targeted vaccines. His laboratory and field-based studies have also served as vital training platforms for over 150 professionals, including physicians, scientists, and public health specialists from around the world.
A recognized leader in the field of global immunization policy, Prof. Cravioto was appointed Chair of the Strategic Advisory Group of Experts (SAGE) on Immunization of the World Health Organization (WHO) from 2015 to 2022, where he helped guide global vaccine policy and implementation strategies during a period of rapid vaccine innovation and deployment. He currently serves as a member of the Gavi Vaccine Investment Strategy 2024 advisory group and WHO’s Product Development for Vaccines Advisory Committee (PDVAC).
In 2025, Prof. Cravioto was invited to join the Technical Advisory Group of Experts on Diseases Preventable by Vaccination for the Pan American Health Organization (PAHO), continuing his long-standing contribution to vaccine policy and regional health security.
Prof. Cravioto is a member of Mexico’s National Academies of Sciences, Medicine, and Pediatrics, and has been honored with honorary professorships from University Ricardo Palma in Peru and University of Cape Town in South Africa, in recognition of his contributions to medical science and public health.
Throughout his career, Prof. Cravioto has combined academic excellence, scientific innovation, and international leadership to address some of the most pressing global health challenges, particularly those affecting vulnerable children in low-resource settings.
Early days
Following in his father’s footsteps, Prof. Cravioto discovered early in his medical career that his passion lay in infectious diseases. He chose to specialize in pediatrics and, by the late 1970s, earned a scholarship to attend the London School of Hygiene and Tropical Medicine. There, he completed a master’s degree in public health followed by a PhD in microbiology, during which he worked on identifying the five main adhesive factors used by enterotoxigenic E. coli to attach to the intestinal lining.
“And those factors, to date, are the basis of the vaccines against E. coli that are being tested and used, which is something that I’m very proud of being able to contribute in that sense to the field,” says Prof. Cravioto.
One of the most significant changes Prof. Cravioto has observed in public health and science education is access to information. He recalls visiting libraries and combing through the massive Index Medicus volumes to see whether a journal had arrived.
In 1995, when he became Dean of the Faculty of Medicine at UNAM, he helped establish three computing centers connected by a fiber optic network, linking various hospitals in Mexico City affiliated with the university. It became one of the few medical schools in the region with internet access.
Landscape on vaccines against Enterobacteriaceae
Enterobacteriaceae, a large family of Gram-negative bacteria, includes several significant pathogens such as Klebsiella, Enterobacter, Citrobacter, Salmonella, Escherichia coli, Shigella, Proteus, Serratia, among others. These organisms are commonly associated with urinary tract infections (UTIs), and some species are also major causes of diarrheal diseases.
Prof. Cravioto’s pioneering research on ETEC and EPEC has been instrumental in deepening scientific understanding of diarrheal diseases and shaping the development of targeted vaccines.
When analyzing global disease burden studies focused on enteric diseases, there has been a notable decrease in diarrheal illnesses worldwide. However, these diseases remain prevalent in countries where access to clean water and proper sanitation is still a challenge. A major turning point came with the widespread introduction of the rotavirus vaccine in the early 2000s, which led to a significant decline in diarrheal cases in urban areas.
He points out that while cholera and enterotoxigenic E. coli (ETEC) require approximately 100,000 organisms to cause disease, this is not the case for pathogens with lower infectious doses, making their transmission routes and public health implications very different.
This manufacturing bottleneck reflects broader challenges in vaccine development and distribution within the Enterobacteriaceae family, including limited R&D funding. The recent decision by the United States to withdraw support for Gavi, the Vaccine Alliance, further complicates the future of vaccine access. This uncertainty casts doubt on how many new vaccines, such as those for RSV or Shigella, will be added to Gavi’s portfolio, and which might be excluded due to resource constraints.
Misinformation vs. evidence
Although global acceptance of vaccination as a vital public health measure remains high, there is a growing segment of the population that expresses hesitancy about vaccinating themselves or their children. Misinformation, combined with a rising mistrust in institutions, plays a significant role in fueling this reluctance.
“The [anti-vaccine] movement in the United States is something that worries us very much because there is now the power to affect a number of [policy] changes that might be very harmful both for the U.S. and for the whole world,” affirms Prof. Cravioto, who notes that due to increasing skepticism and ethical concerns, conducting phase three placebo-controlled trials has now become nearly impossible in many contexts.
Prof. Cravioto sustains that the WHO’s Strategic Advisory Group of Experts (SAGE) on Immunization looks at the evidence for each recommended vaccine in an utmost thorough way. He explains that the evidence is not just analyzed but graded. But the critical question remains: how strong is the evidence to support a decision?
To determine the strength of the evidence, SAGE uses a highly structured and transparent process known as the GRADE approach –Grading of Recommendations, Assessment, Development and Evaluation. This process ensures that recommendations are grounded in best available science, while also considering public health realities.
After this evidence is thoroughly analyzed, a technical working group drafts recommendations, which are then presented to the 15-member advisory group. Following internal deliberations and final approval, the recommendation is passed on to the WHO Director-General and ultimately becomes WHO policy.
“The system is set up to create confidence and I don’t think we talk about it enough,” he emphazises.
WHO protocols during the pandemic
As Chair of SAGE during the COVID-19 pandemic, Prof. Cravioto faced unprecedented challenges and responsibilities. Unlike previous vaccine evaluations, the urgency and scale of the crisis required a much larger and more agile response.
To meet the moment, SAGE expanded its working group, which met three times a week via Zoom, to include key stakeholders. They brought in the head of the WHO Product Development Committee, vaccine regulators responsible for approval pathways, and the chairs of the regional advisory groups of the five regional WHO offices. This structure allowed real-time feedback on how proposed recommendations would function in different parts of the world. It also ensured direct collaboration with the U.S. Centers for Disease Control and Prevention (CDC), and other organizations.
Importantly, SAGE decided not to exclude vaccine manufacturers from the process. By working closely with the producers, a major departure from traditional practice normally done through independent working groups, they were able to recommend 13 new vaccines for emergency use during the pandemic. Industry had a place in the room, invited to the conversation to present their data, yet not as active participants in the discussions.
This early and open engagement gave the working group critical insights into the progress of clinical trials, enabling them to recommend the inclusion of essential elements for data collection and safety monitoring, information needed to make sound policy decisions in real time.
Prof. Cravioto believes one of the group’s greatest successes was fostering trust among all stakeholders which, up to that moment of intense global uncertainty, had been unattainable.
“And then, of course, the world was able to accept our recommendations,” he commends.
WHO challenges
In today’s politically and ideologically polarized world, one of the WHO’s most pressing challenges is funding. While it is clear that traditional models and institutional frameworks must evolve to meet modern global health needs, Prof. Cravioto emphasizes that organizations like the WHO must continue to uphold the founding principles and the outstanding legacy of public health work built over decades.
Due to budget constraints, the SAGE committees involved in vaccine development, safety, policy, and pipeline evaluation can no longer meet in person. While committee members work voluntarily, the cost of managing the full process, from reviewing data to producing official position papers, is significant.
“The amount of work that can be done is [directly] correlated to the amount of funds you have,” he notes.
Transparency and integrity remain central to SAGE’s operations. Every committee member is vetted for conflicts of interest. During the COVID-19 pandemic, five of the 15 members were actively involved in vaccine research. Although they were allowed to contribute to discussions due to their expertise, they were excluded from decision-making. Prof. Cravioto stresses the importance of this practice.
He warns that halting key institutional functions due to funding cuts has long-term consequences. Research pipelines, expert collaboration, and institutional memory are all at risk -and these aren’t easily rebuilt once lost. The loss of skilled human capital and program continuity is particularly damaging.
Prof. Cravioto argues that by defunding the WHO, countries -particularly the United States- risk losing both influence and alignment with global health strategies.